Vaccines
- Vaccines prevent or mitigate infections.
- They are designed to induce a protective immune response in the body against the viruses.
- When vaccinated, the immune system of the body produces a specific response, consisting of specific T cells & specific antibodies that fight off the infection when exposed to the virus occurs at a later stage.
- More importantly, vaccination also leads to the induction of a specific immunological memory against the viruses represented in the vaccine.
- There are about a half-dozen basic types of vaccines, including killed viruses, weakened viruses, & parts of viruses, or viral proteins.
- All aim to expose the body to components of the virus so specialized blood cells can make antibodies.
- In the past, it has been difficult to manufacture vaccines for new zoonotic diseases quickly.
- A lot of trial & error is involved in making a vaccine. Hence it could take years to invent a vaccine.
- A new approach being taken by Moderna Pharmaceuticals, which recently began clinical trials of a vaccine, is to copy genetic material from a virus & add it to artificial nanoparticles.
- This makes it possible to create a vaccine based purely on the genetic sequence rather than the virus itself.
Differences between Vaccine & Drugs
Vaccines | Drugs |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Antiviral treatments for COVID-19
Antivirals
Antibiotics
|
- Antiviral treatments use various tactics to slow down the virus’s spread, though it is not yet clear how effective any of these are.
- Chloroquine & hydroxychloroquine, typically used to fight malaria, might inhibit the release of the viral RNA into host cells.
- Favipiravir, a drug from Japan, could keep viruses from replicating their genomes.
- Combination therapy of lopinavir & ritonavir, a common HIV treatment that has been successful against MERS, prevents cells from creating viral proteins.
- Some believe the ACE2 protein that the coronavirus latches onto could be targeted using hypertension drugs.
- Another promising approach is to take blood serum from people who have recovered from the virus & use it & the antibodies it contains as a drug.
- It could be useful either to confer a sort of temporary immunity to health-care workers or to combat the virus’s spread in infected people.
- This approach has worked against other viral diseases in the past, but it remains unclear how effective it is against SARS-CoV-2.
Major Vaccines in News in the context of COVID-19
What is ZyCoV–D?
- ZyCoV-D is a plasmid DNA vaccine, under the Vaccine Discovery Programme supported by the Department of Biotechnology under the National Biopharma Mission.
- Plasmids are circular deoxyribonucleic acid (DNA) vectors that can be used as vaccines to prevent various types of diseases.
- In the pre-clinical phase, the vaccine was found to elicit a strong immune response in multiple animal species like mice, rats, guinea pigs & rabbits.
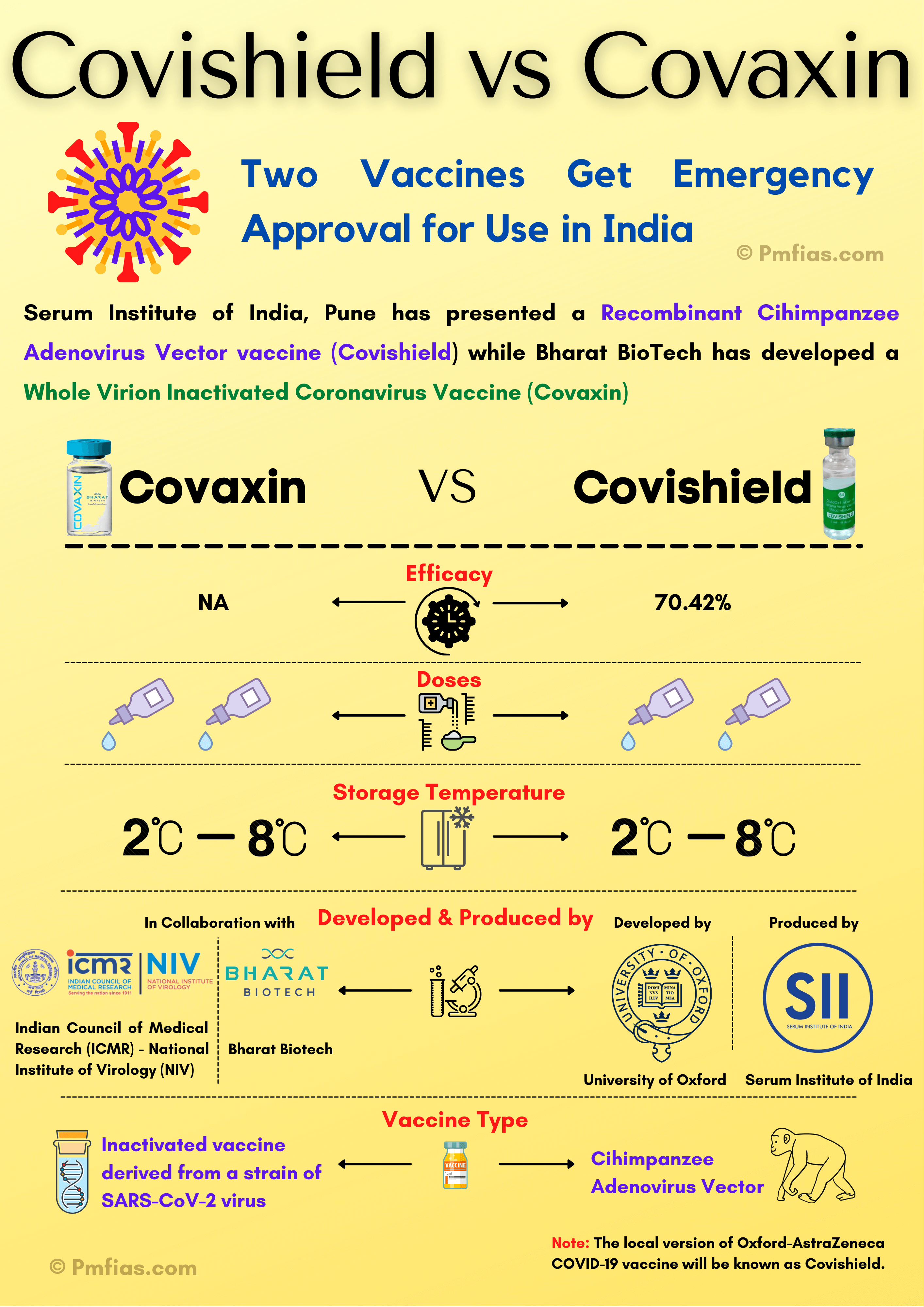
What is Oxford’s ChAdOx1 Covid–19 vaccine?
- Vaccine, based on a chimpanzee adenovirus called ChAdOx1, elicited antibody & T-cell immune responses.
- Oxford’s AZD1222 vaccine is made from a genetically engineered virus that causes the common cold in chimpanzees.
What is COVAXIN?
- It has been developed by the company Bharat Biotech India (BBIL) in collaboration with ICMR’s National Institute of Virology (NIV).
- It is an “inactivated” vaccine — one made by using particles of the Covid–19 virus that were killed, making them unable to infect or replicate, ie non replicating.
- Injecting particular doses of these particles serves to build immunity by helping the body create antibodies against the deadly virus.
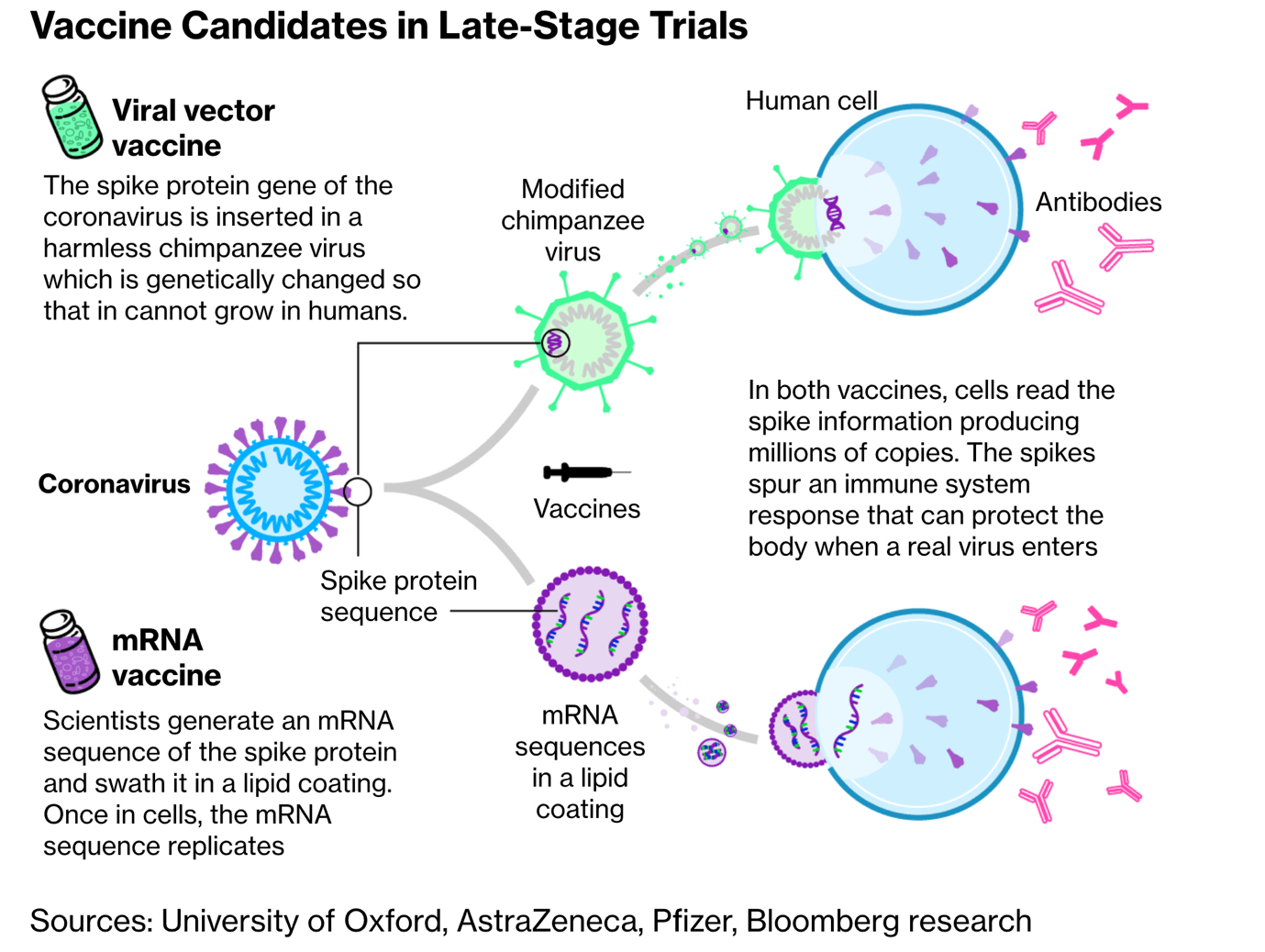
What is Non–Replicating Viral Vector?
- The SARS–CoV–2 virus uses the spike on its surface, the ‘spike protein’, to enter & infect cells & multiply.
- A non–replicating viral vector vaccine uses a weakened version of a different virus to carry this Covid–19 spike protein into the body, but it is modified not to replicate.
What is the mRNA vaccine?
RNA Vaccine | DNA Vaccine |
|
|
- The genetic blueprint (or code) in living organisms is stored in a double-stranded molecule called DNA (deoxyribonucleic acid), which makes proteins that are responsible for nearly every function in the human body.
- The conversion of DNA code into proteins requires a single-stranded molecule called the mRNA (messenger ribonucleic acid).
- In an analogy with computers, one may think of the DNA as the hardware, the mRNA as the software & proteins as the applications.
- The mRNA-1273 is a piece of RNA that carries the code to make the COVID-19 virus Spike protein when introduced into cells.
- This protein present on the virus surface is critical for its entry into cells. Immunity (antibodies) to the Spike protein can block virus entry & its multiplication, & thus ameliorate the disease.
Sputnik-V
- This vaccine has been developed by Moscow’s Gamaleya Institute in collaboration with Russia’s defence ministry.
- The vaccine is based on the DNA of a SARS-CoV-2 type adenovirus, a common cold virus.
- In this vaccine, adenovirus is used as a tool to deliver genes or vaccine antigens to the target host tissue.
- The vaccine uses the weakened virus to deliver small parts of a pathogen & stimulate an immune response.
- The vaccine is administered in two doses & consists of two types of human adenovirus, each carrying an S-antigen of the new coronavirus, which enter human cells & produce an immune response.
Which is the Best Vaccine Suited for India?
- Comparing the top three vaccines based on:
Efficacy Rates
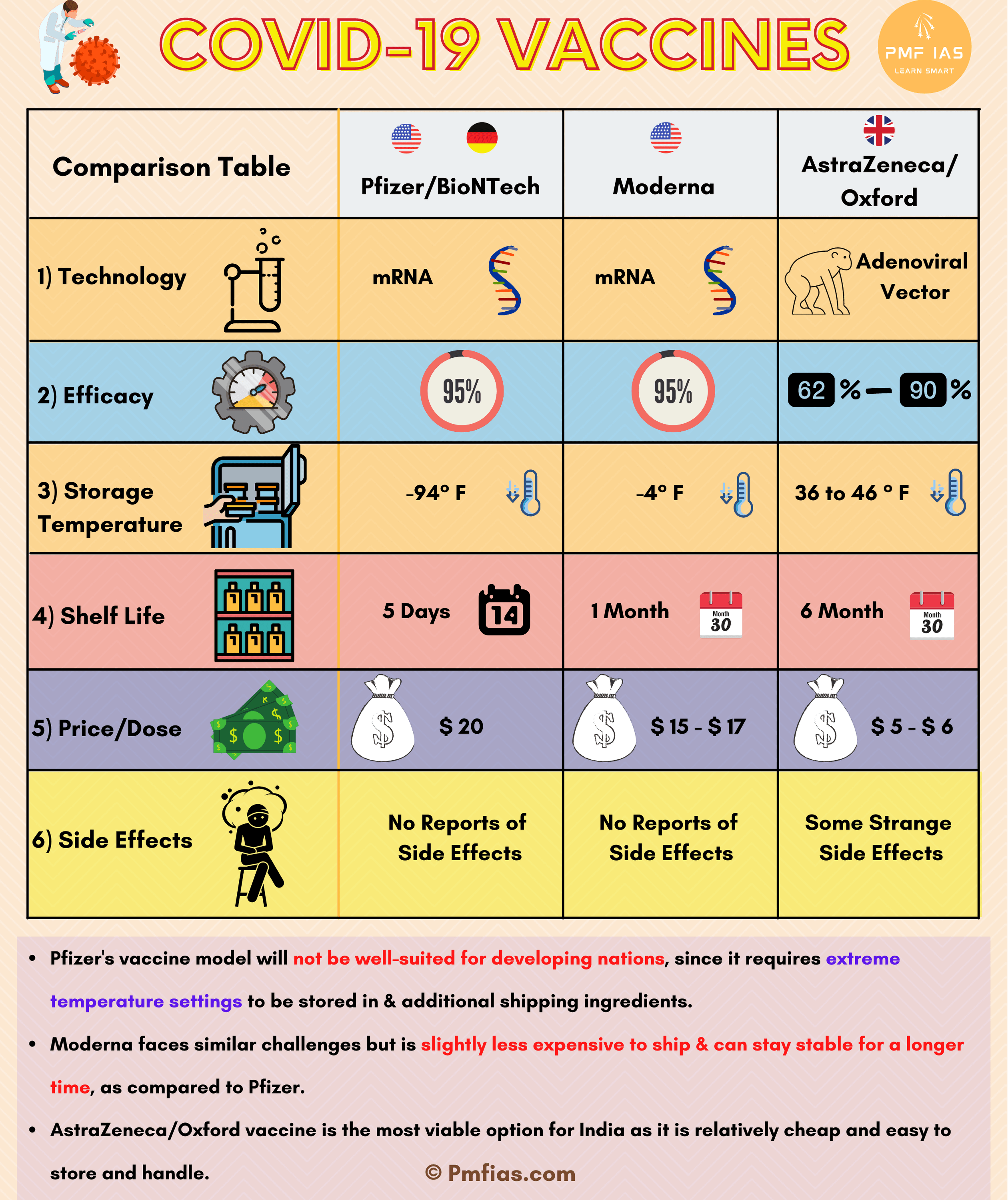
Pricing
- Pfizer’s candidate is the steepest one right now, costing $20 per dose.
- Moderna’s make comes up to cost somewhere around $15-$17 per dose.
- Oxford-Astrazeneca’ shot is by far the cheapest vaccine under offering, as little as $5- $6 (Rs.1000).
Side Effects
- Both Moderna & Pfizer-BionTech haven’t reported the occurrence of undue or alarming side-effects.
- Neither have reports of adverse reactions emerged from people who have been vaccinated right now.
- In comparison to this, the Oxford-Astrazeneca vaccine has been surrounded by controversies in the past months with the many ‘strange’ side-effects being reported from volunteers
Storage & shelf-life
- Storage & shelf-life are prime factors that determine how effective a vaccine would be in real-world settings.
- Many experts claimed that Pfizer’s vaccine model will not be well-suited for developing nations, since it requires extreme temperature settings to be stored in & additional shipping ingredients.
- The vaccine can be stored for use for up to 5 days’ time in a regular refrigerator, for 30 days in a dry-ice freezer, or 6 months’ time in ultra-cold freezers, which are not feasible to arrange everywhere.
- Moderna faces similar challenges but is slightly less expensive to ship & can stay stable for a longer time, as compared to Pfizer.
- Oxford’s dose, wins since it is a vaccine prepared using traditional settings, can be stored for use for longer months, easily delivered & administered.
Important Drugs in News in the context of COVID-19
What is Itolizumab?
- This was used for treating chronic plaque psoriasis.
- Plaque psoriasis is a chronic autoimmune condition in which skin cells build up & form scales & itchy, dry patches.
- It can also be used in the treatment of CRS in moderate to ARDS in severely affected patients of the corona.
- CRS (cytokine release syndrome) & ARDS (acute respiratory distress syndrome) happen due to COVID–19 suffering.
- CSS is an uncontrolled attempt by the immune system to neutralise the virus that often ends up damaging the lungs & other organs & even death.
- ARDS is a disease in which the lung loses its capacity to expand further.
- Biocon’s biomanufacturing facility which is located at Biocon Park in Bengaluru will be manufacturing & formulating Itolizumab as an intravenous injection.
- Biocon has licensed Itolizumab from Cuba twenty years ago & this is an original innovative Indian drug.
What is Hydroxychloroquine?
- It is a drug used in the treatment of autoimmune diseases such as rheumatoid arthritis & lupus.
- Hydroxychloroquine (HCQ) is also used for the prevention of malaria & its treatment; it is a derivative of the antimalarial drug chloroquine.
- Hydroxychloroquine can only be used in places where chloroquine is still effective.
- There are only a few places left in the world where hydroxychloroquine is still effective including parts of Central America & the Caribbean.
Hydroxychloroquine: Why is it so much in the spotlight?
- The prime mover of the theory that HCQ works against Covid–19 has been President Trump, starting with his tweet in March: “HYDROXYCHLOROQUINE & AZITHROMYCIN (antibiotic), taken together, have a real chance to be one of the biggest game-changers in the history of medicine.
What is Dexamethasone?
- Dexamethasone reduces the production of the chemicals that cause inflammation & also reduces the activity of the immune system by affecting the way white blood cells function.
- Dexamethasone falls in a category called corticosteroids, which closely mimic cortisol, the hormone naturally produced by the adrenal glands in humans.
- It is commonly used in treatment for rheumatological inflammatory conditions: inflammations of muscles, inflammation of blood vessels, chronic arthritis, & lupus.
- It is used in lung diseases, kidney inflammation & eye inflammation, & to reduce swelling associated with tumours of the brain & spine.
- In cancer patients, it is used to treat nausea & vomiting caused by chemotherapy drugs.
How Useful is it in Covid–19 Treatment?
- During the SARS outbreak in 2003, corticosteroid therapy was used to reduce inflammatory–induced lung injury.
- In Covid–19, too, many countries are investigating the effectiveness of corticosteroid therapy on patients with an acute respiratory infection.
- Also, the World Health Organization (WHO) has prioritised the evaluation of corticosteroids in clinical trials to assess safety & efficacy.
What is Remdesivir?
- Its an antiviral drug being used to treat COVID–19 patients.
- Remdesivir is designed to obstruct the stage of replication, when the virus creates copies of itself, followed endlessly by the copies creating copies of themselves.
- Polymerase enzyme is targeted by remdesivir
How does replication take place?
- Once the virus enters the human cell, it releases its genetic material, which is then copied using the body’s existing mechanism.
- At the replication stage, the key viral protein at play is an enzyme called RdRp (an enzyme is a kind of protein that speeds up chemical reactions within a cell).
- It is RdRp that makes the copies, by processing components of the RNA of the virus.
- In scientific literature, such an enzyme is called a polymerase (the p is RdRp stands for polymerase) or a replica. In any case, this is the enzyme that is targeted by remdesivir.
How exactly does remdesivir target this enzyme?
- In order to replicate, the copy machine processes raw material from the virus RNA, broken down by another enzyme with that specific function.
- When a patient is given remdesivir — the inhibitor — it mimics some of this material, & gets incorporated in the replication site.
- With remdesivir replacing the material it needs, the virus fails to replicate further.
How far has this action been established?
- The drug itself was designed to act against the Ebola virus, which is not a coronavirus.
Favipiravir
- Favipiravir is an antiviral given to inhibit viral replication.
- It is used as an anti-influenza drug.
- It is being used for moderately symptomatic to severely ill Covid patients, but access is not easy.
Plasma Therapy
What is Plasma?
- Plasma is the almost–clear liquid left behind after RBCs; WBCs & platelets are removed from the blood.
- Plasma fluid carries the blood components throughout the body.

Link– Source & Credits
- Plasma is the largest part of your blood. It makes up more than half (about 55%) of its overall content.
- When separated from the rest of the blood, plasma is a light–yellow liquid.
- Plasma carries water, salts & enzymes.
- The main role of plasma is to take nutrients, hormones, & proteins to the parts of the body that need it.
- Cells also put their waste products into the plasma.
- The plasma then helps remove this waste from the body.
What is Convalescent Plasma Therapy?
- Convalescent plasma therapy is an experimental treatment that some doctors are using for people with severe coronavirus disease in 2019 (COVID–19).
- People who’ve recovered from COVID–19 have antibodies — proteins the body uses to fight off infections — to the disease in their blood.
- The blood from people who’ve recovered is called convalescent plasma.
- Researchers hope that convalescent plasma can be given to people with severe COVID–19 to boost their ability to fight the virus.
- It also might help keep people who are moderately ill from becoming more ill & experiencing COVID–19 complications.

Link– Source & Credits
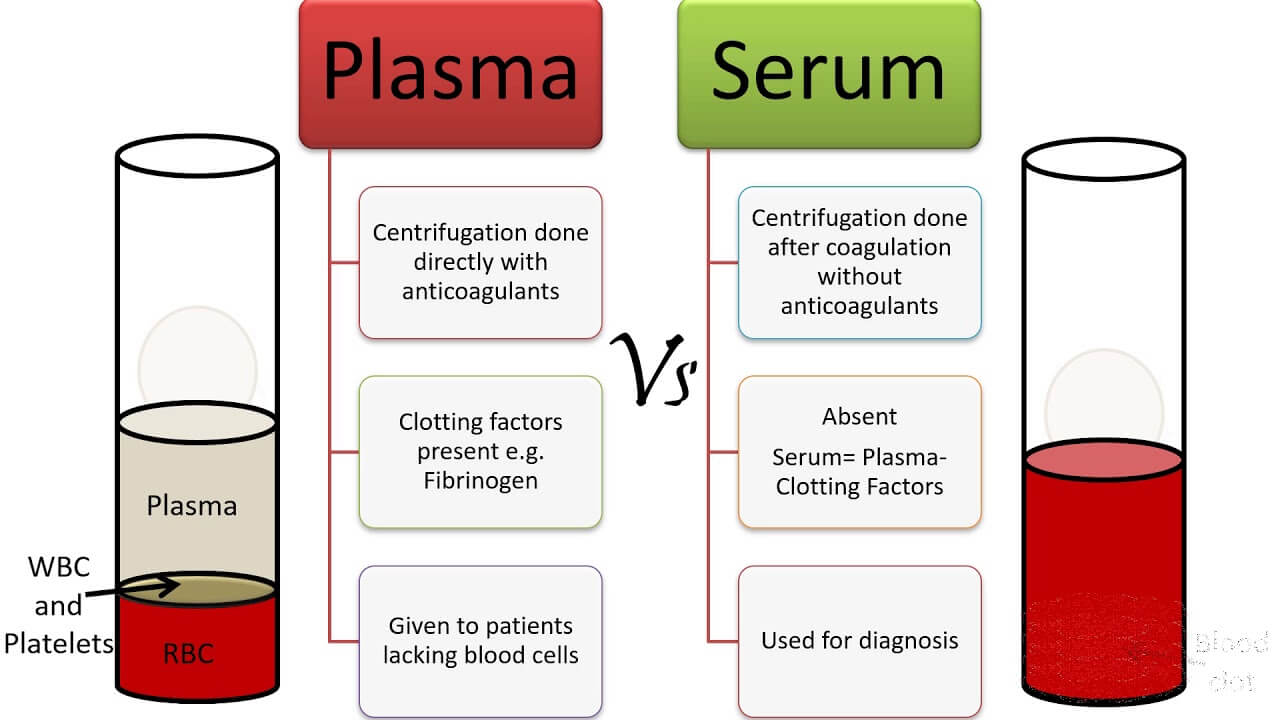
Plasma vs Serum
- Serum is plasma minus the clotting factors & blood cells.
- While removing the clotting factors (by centrifugation), the protein fibrinogen is converted to fibrin.
- Fibrin is an insoluble protein that is used to assist in the repair of tissue damage by forming a clot.
- A key difference between plasma & serum is that plasma is liquid, & serum is fluid.
- Plasma contains fibrinogen which is absent in serum.
- Both plasma & serum can be extracted from blood but it’s worth noting that serum is obtained after the clotting of blood, while plasma can be obtained before the coagulation of the blood.
- Serum is mostly used for blood typing but is also used for diagnostic testing.
- Plasma, on the other hand, is mostly used for blood-clotting related problems.



0 Comments